Vitamin D3 deficiency continues to be one of the most persistent and unresolved nutritional challenges worldwide. Despite widespread testing, frequent prescriptions, and repeated high-dose supplementation, achieving and maintaining vitamin D adequacy remains elusive—particularly in India and across Asia.
As we move into 2026, clinicians are reassessing long-standing practices and asking a critical question:
Is daily vitamin D3 supplementation superior to weekly or bolus dosing for both prevention and therapy?
And more importantly, does liposomal vitamin D3 daily dosing offer a meaningful clinical advantage in real-world practice?

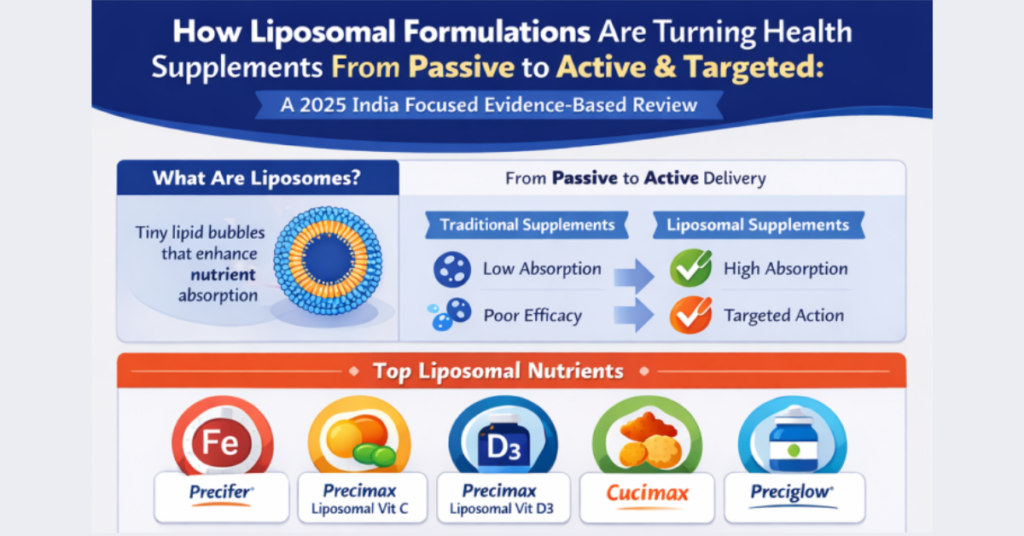
This evidence-based review examines daily versus weekly vitamin D3 dosing, why deficiency persists, how testing strategies fail, and how liposomal vitamin D3 (Precimax Liposomal Vitamin D3 capsules) is redefining consistency, adequacy, and long-term outcomes.
Vitamin D3 Deficiency: India, Asia, and the Global Burden
Vitamin D deficiency is no longer restricted to cold climates. Paradoxically, it is highly prevalent in sun-rich regions.
Reported prevalence (approximate):
- India:70–90% of adults; high prevalence even in children
- Asia:60–80%
- Middle East:60–90%
- Europe:40–60%
- North America:30–50%
Deficiency is documented in:
- Apparently healthy adults
- Athletes and physically active individuals
- Elderly populations
- Children and adolescents
Low vitamin D status is consistently associated with:
- Osteoarthritis and chronic joint pain
- Osteoporosis and fracture risk
- Diabetes and insulin resistance
- Cardiovascular disease and stroke
- Autoimmune disorders
- Recurrent infections
These associations underscore why vitamin D3 sufficiency is not optional—it is foundational to long-term health.
Why Vitamin D3 Sufficiency Continues to Elude Patients
Despite frequent supplementation, many patients fail to achieve or maintain adequate serum 25-hydroxy vitamin D [25(OH)D] levels. The reasons are systemic, not individual.
Key contributors include:
- Over-reliance on weekly or bolus dosing without maintenance
- Ignoring absorption and delivery mechanisms
- Inconsistent laboratory monitoring
- Use of unstable or unproven supplement formats
- Lack of attention to cofactors such as magnesium
As a result, vitamin D therapy often becomes episodic rather than physiological.
Daily vs Weekly Vitamin D3 Dosing: What Current Evidence Shows
Weekly (Bolus) Vitamin D3 Dosing
Weekly regimens (commonly 60,000 IU) are widely used to correct deficiency quickly. They are effective for short-term correction, especially in severe deficiency.
However, clinical limitations are well recognized:
- Wide fluctuations in serum levels
- Peak-and-trough physiology
- Poor adherence after correction
- Patients often stop supplementation once “numbers improve”
Weekly dosing corrects deficiency, but rarely ensures long-term adequacy.
Daily Vitamin D3 Supplementation
Daily dosing (1,000–4,000 IU/day) more closely mimics endogenous vitamin D synthesis from sunlight.
Comparative clinical studies show:
- Daily dosing is as effective as weekly dosingin achieving sufficiency
- Serum levels are more stable over time
- Better adherence and fewer overshoots

Clinical implication:
Weekly dosing may correct deficiency, but daily dosing sustains adequacy—provided absorption is reliable.
Why Vitamin D3 Test-Based Approaches Often Fail
A major reason vitamin D therapy underperforms is inconsistent testing strategy.
Common issues include:
- Baseline testing without post-treatment follow-up
- Switching laboratories between tests
- Testing in different seasons
- Inadequate intervals between dose and blood draw
Best practices for predictable results:
- Use the same laboratory consistently
- Test at similar times of year
- Re-check 8–12 weeks after starting or changing dose
- Monitor again during maintenance
Dr. Jagannath, Head Pathologist at Truecare Diagnostics, Bangalore, reports that structured repeat-testing packages significantly improve interpretation of vitamin D trends and guide rational dosing decisions.

How to Interpret 25-Hydroxy Vitamin D3 Levels Clinically
25(OH)D Level (ng/mL) | Interpretation |
<20 | Deficiency |
20–30 | Insufficiency |
30–50 | Adequate (general health) |
50–70 | Optimal |
70–100 | Target for chronic & high-risk conditions |
Increasingly, clinicians aim for 70–100 ng/mL in:
- Osteoarthritis
- Osteoporosis
- Autoimmune disorders
- Chronic musculoskeletal pain
- Recurrent infections
Vitamin D3 Supplement Formats: Why Form Matters
Vitamin D3 is available as:
- Weekly sachets (powders)
- Weekly softgels
- Daily tablets or capsules
- Daily sachets
- Gummies, chewables, effervescents
Why gummies, chewables, and effervescents can be avoided
These formats often suffer from:
- Poor stability
- Variable dosing
- Sugar or excipient burden
- Unpredictable absorption
They may improve palatability—but not clinical outcomes.
Liposomal Vitamin D3 Daily Dosing: A Breakthrough in Consistency
Liposomal delivery encapsulates vitamin D3 in phospholipid vesicles, enhancing:
- Intestinal absorption
- Cellular uptake
- Bioavailability at lower doses
- Stability of serum levels
Precimax Liposomal Vitamin D3 capsules are designed for daily physiological dosing, particularly beneficial in:
- Elderly individuals
- Obesity
- Diabetes
- Thyroid and autoimmune disorders
- Patients with plateaued vitamin D levels
Real-world clinical experience
Dr. Anna Travesco, Family Physician, Mumbai, reports using Precimax Liposomal Vitamin D3 for over three years in 300+ patients, noting:
- More predictable achievement of adequacy
- Reduced need for repeated bolus dosing
- Better patient compliance
- Stable maintenance over time
Dr. V.R. Ram, Coimbatore, adopts a hybrid strategy—weekly correction followed by daily liposomal vitamin D3 (Precimax) for maintenance—especially in thyroid disorders, autoimmune diseases, and chronic musculoskeletal conditions.

Magnesium: The Essential Cofactor for Vitamin D3 Effectiveness
Vitamin D activation is magnesium-dependent. Without adequate magnesium:
- Conversion of vitamin D is impaired
- Muscle pain and cramps may worsen
- Clinical response remains suboptimal
This explains why combinations such as liposomal vitamin D3 with liposomal magnesium (e.g., Precimax Liposomal MGD3) often produce superior tolerance and outcomes.
Does Vitamin D Fortification Work?
Food fortification contributes marginally to intake but:
- Provides inconsistent doses
- Rarely corrects deficiency
- Cannot replace targeted supplementation
Fortification is supportive, not therapeutic.
Should Vitamin D3 Be Taken Lifelong or Cyclically?
Evidence supports a cyclic-maintenance approach:
- Correct deficiency (8–12 weeks)
- Maintain with daily physiological dosing
- Monitor periodically (1–2 times/year)
- Adjust dose—not format
Lifelong awareness is essential; lifelong megadosing is not.

Practical Vitamin D3 Strategy for 2026
Correction phase:
Weekly dose or daily liposomal vitamin D3 (based on severity)
Maintenance phase:
Daily liposomal vitamin D3 + magnesium adequacy
Monitoring:
Consistent lab, consistent timing, trend-based decisions
image
FAQs
- Is daily vitamin D3 supplementation better than weekly dosing?
Both daily and weekly regimens have advantages and limitations. However, when a medical condition requires achieving and maintaining higher serum vitamin D3 levels, a hybrid approach—initial correction with weekly dosing followed by daily liposomal vitamin D3 for maintenance—is often more effective and sustainable.
- Why do vitamin D levels fall after stopping weekly sachets?
Weekly sachets correct deficiency temporarily but do not create adequate tissue reserves. Once stopped, serum levels fall rapidly in the absence of maintenance dosing.
- Is liposomal vitamin D3 better absorbed than regular vitamin D3?
Yes. Liposomal vitamin D3 is better absorbed and less dependent on fat digestion, bile secretion, or gut integrity, unlike conventional fat-soluble vitamin D3 formulations.
- What is the ideal vitamin D3 level for chronic conditions?
For chronic conditions, most clinicians now aim for a serum 25-hydroxy vitamin D level of 70–100 ng/mL, under medical supervision.
- Why is magnesium necessary with vitamin D3?
Magnesium is essential for the activation, transport, and utilization of vitamin D3. Without adequate magnesium, vitamin D3 supplementation often produces suboptimal results.
- Can vitamin D gummies be trusted?
Vitamin D gummies are not ideal for therapeutic correction. They may be used as a fortification option, but added sugar content, inconsistent dosing, and uncertain stability limit their clinical usefulness.
- Does obesity affect vitamin D response?
Yes. Obesity significantly reduces vitamin D bioavailability due to sequestration in adipose tissue, often requiring higher or more bioavailable formulations.
- How often should vitamin D testing be repeated?
Testing should be done using a reliable, accredited laboratory, ideally at a fixed time of year. Repeat testing is usually recommended 8–12 weeks after therapy initiation or dose change, and thereafter as advised by the healthcare provider.
- Is daily vitamin D3 safe for long-term use?
Yes. Daily physiological dosing of vitamin D3 is safe for long-term use, especially when monitored periodically.
- Can elderly patients take daily vitamin D3?
Yes. In fact, elderly individuals often require more consistent vitamin D3 supplementation due to reduced synthesis and absorption. Liposomal vitamin D3 is particularly suitable in this population.
- Is food fortification enough to prevent vitamin D deficiency?
Fortification may provide supportive intake, but there is no strong clinical evidence that fortification alone can correct or prevent deficiency in most individuals.
- Can sunlight alone maintain vitamin D adequacy?
For most people, sunlight alone is insufficient. Adequate vitamin D status requires cofactors, appropriate diet, and often supplementation, especially in modern lifestyles.
- Why do some patients plateau despite supplementation?
Common reasons include absence of cofactors (especially magnesium), missed doses, inadequate dosing, poor absorption, or inappropriate formulation.
- Does liposomal vitamin D3 reduce dose requirements?
Currently, there is limited comparative dose-reduction data. However, liposomal vitamin D3 allows better absorption at lower doses, improving consistency and response.
- Can vitamin D3 help joint pain?
Yes. Multiple studies have shown a direct association between vitamin D deficiency and musculoskeletal pain, and correction often improves symptoms.
- Is weekly dosing still useful?
Yes. Weekly dosing can be useful during the initial correction phase, especially under medical supervision.
- What causes vitamin D toxicity?
Vitamin D toxicity is rare and usually results from excessive dosing over long periods, often combined with lack of monitoring and inadequate cofactors, rather than normal supplementation.
- Should the same lab be used for repeat testing?
Yes. Using the same accredited laboratory improves consistency and allows more reliable interpretation of trends.
- Can vitamin D3 support diabetes management?
Yes. Adequate vitamin D3 status supports insulin sensitivity and metabolic health, though it does not replace standard diabetes treatment.
- What is the biggest reason vitamin D therapy fails?
Vitamin D therapy usually fails due to poor absorption, inappropriate formulation, inadequate duration, inconsistent dosing, or lack of cofactors. Rarely is a single factor responsible.