At the recent ETHealthworld Conclave in New Delhi, clinicians from endocrinology, orthopaedics, pediatrics, trauma care and public health came together to spotlight a reality that has flown under the radar for too long in Indian healthcare: bone health is a lifelong concern, not something to be addressed only after a fracture. Experts emphasized that fractures, osteoporosis, and fragile bones are not inevitable consequences of ageing — they are largely preventable with early action and integrated care strategies.
In a country with rapidly ageing demographics, widespread nutritional gaps, high prevalence of lifestyle risk factors (such as low sun exposure and sedentary habits), and significant rural–urban disparities, the need for a lifelong bone health strategy is urgent. This health imperative spans life stages from toddlers and adolescents building peak bone mass to adults seeking metabolic resilience and older adults aiming to prevent debilitating fractures.
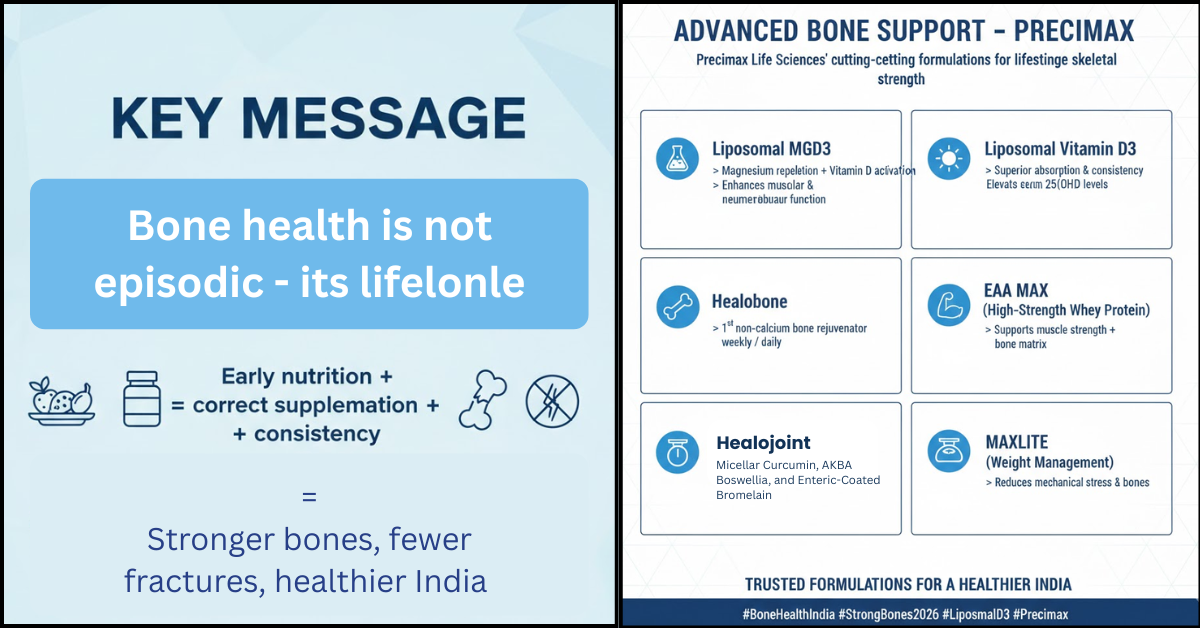
This blog synthesizes the conclave’s key messages and blends them with cutting-edge, India-applicable approaches including nutraceutical support with advanced formulations — such as Precimax Liposomal MGD3, Precimax Liposomal Vitamin D3, Healobone (micronized Cissus quadrangularis + liposomal vitamin D3 + K2-7), EAA MAX high-strength whey protein, and MAXLITE for weight loss. These formulations can be strategic allies in building and maintaining robust bones throughout life.
India’s Bone Health Challenge: A Life-Course Problem
Experts at the conclave underscored that bone health is a continuum, beginning in early life and extending into old age. Dr. Nitin Kapoor (endocrinologist) highlighted a key biological fact: peak bone mass is typically achieved by about 30 years of age. Building a high peak bone mass in childhood and adolescence dramatically reduces the risk of osteoporosis and fractures later in life, yet many Indian children have low bone density due to inadequate nutrition and lifestyle factors.
Dr. Chetan Pradhan (trauma expert) highlighted another critical risk factor: sedentary lifestyles and increased screen time in children are eroding opportunities for weight-bearing activities that stimulate bone formation during the crucial early years.
Equally concerning is data from population studies showing that lifestyle factors like sunlight exposure, tobacco use, rural versus urban residence, and physical activity significantly influence bone health outcomes in Indian adults. For example, osteoporosis prevalence among adults in rural Indian women is substantially higher than in urban cohorts, with sunlight exposure and lifestyle factors directly impacting bone density.
Bone Health Is Not Only About Calcium and Vitamin D
Many Indians still associate bone strength primarily with calcium and occasional vitamin D supplementation, but evidence and clinician experience show bone health is far more complex.
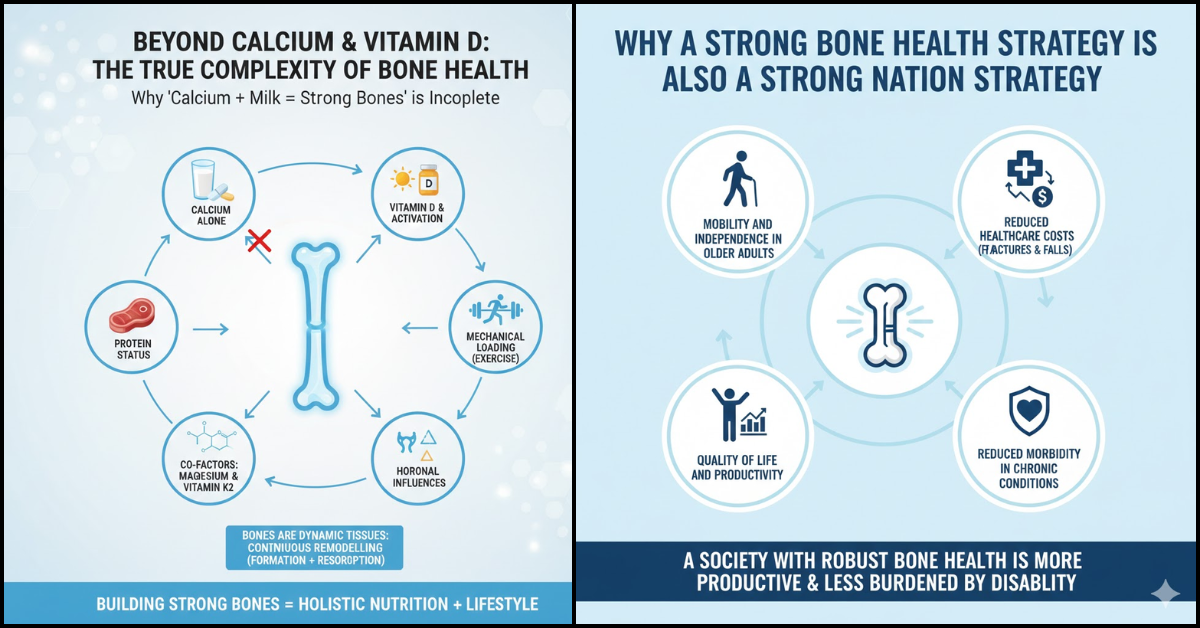
Why “Calcium + Milk = Strong Bones” Is Incomplete
Traditional narratives like “drink milk to prevent bone loss” mislead by oversimplifying bone biology. Bones are dynamic tissues that undergo continuous remodelling throughout life, with both formation and resorption happening simultaneously. A focus on calcium alone ignores critical factors like:
- vitamin D and its activation
- protein status
- hormonal influences
- mechanical loading (exercise)
- co-factors like magnesium and vitamin K2
Moreover, calcium supplementation alone — especially without adequate vitamin D, magnesium, and mechanical stimulation — may not translate into improved bone quality.
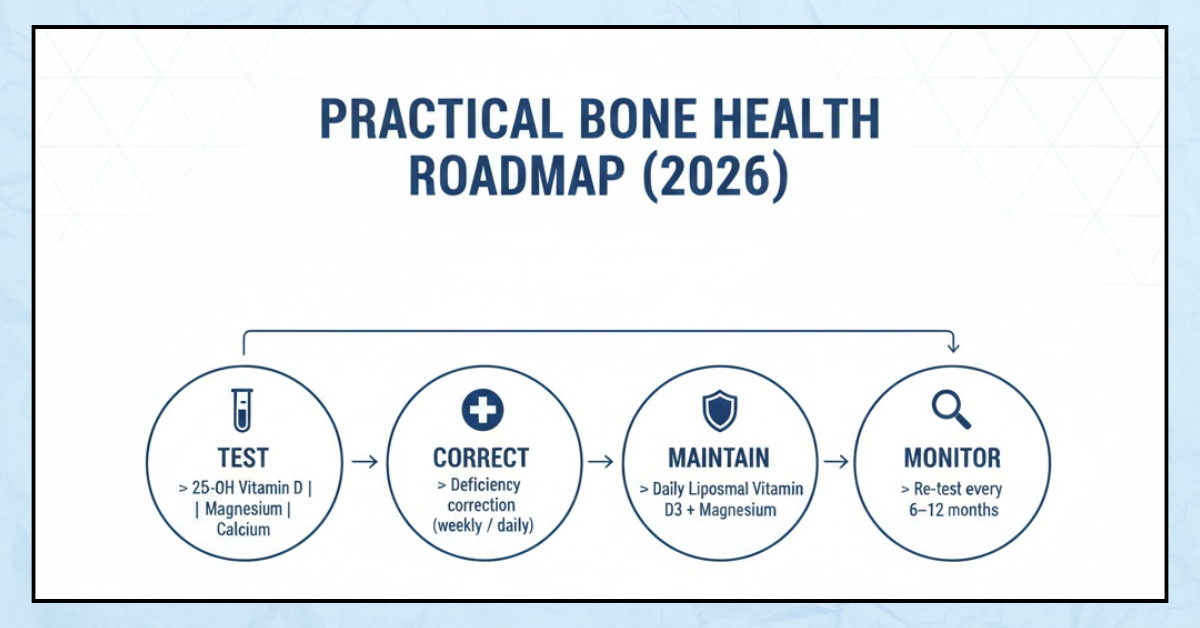
Beyond Baseline Lab Testing
Clinicians at the conclave also underscored a prevalent clinical gap: bone health assessments often occur only after a fracture. Dr. Sunil Marwah (orthopaedic surgeon) warned that nearly 80 % of fracture patients are treated for the fracture itself without addressing the underlying bone fragility that predisposed them to injury.
Experts recommended periodic bone density assessments (such as DEXA scans) and validated risk calculators (e.g., FRAX) for older adults and those with diabetes to complement laboratory testing. Early risk detection, paired with targeted interventions, can reduce future fracture risk.
image
Lifelong Bone Health by Life Stage: Where Nutraceutical Support Fits In
A lifelong strategy requires interventions at every stage of life micro-cycle. Precimax’s advanced formulations offer evidence-aligned support across these life stages.
Childhood & Adolescence: Building Peak Bone Mass
Peak bone mass underpins lifelong skeletal resilience. Nutrition during these years should combine:
- Balanced protein intake
- Calcium-rich foods (dairy, ragi, almonds, leafy greens)
- Regular outdoor play in daylight
- Formulations that support micronutrient sufficiency
While sunlight and habits are foundational, nutraceutical support geared toward enhanced absorption and co-factor synergy can bolster dietary intake when gaps exist.
Adulthood: Maintenance and Prevention
Once peak bone mass is achieved, the focus shifts to maintenance and prevention of accelerated loss due to factors such as:
- Sedentary lifestyle
- Metabolic disorders like diabetes
- Suboptimal nutrient intake
- Hormonal fluctuations
Here, formulations like:
- Precimax Liposomal Vitamin D3— enhances vitamin D3 absorption through liposomal delivery, which bypasses typical fat-dependency hurdles of conventional supplements
- Precimax Liposomal MGD3— restores magnesium status, a co-factor essential for vitamin D activation and bone metabolism
play a crucial role in preventing gradual bone deterioration.
Midlife and Beyond: Supporting Bone Remodelling
In midlife — especially for women post-menopause and older adults — bone remodelling shifts toward net loss, increasing osteoporosis risk. At this stage:
- Healobone(a non-calcium based bone rejuvenator): Combines micronized Cissus quadrangularis with liposomal vitamin D3 and vitamin K2-7.
- Cissus quadrangularishas been traditionally used to support bone healing and structural integrity.
- Vitamin K2-7 helps direct calcium to bone matrix rather than soft tissues, aiding bone mineralization.
- EAA MAX high-strength whey proteinsupports muscle health and amino acid availability, crucial because muscle strength and bone health are synergistic; strong muscles reduce fall and fracture risk.
- MAXLITE Weight-Loss Formulationsupports metabolic health and reduces adiposity — an important component because obesity is linked with lower bone quality and altered load mechanics that paradoxically increase fracture risk.
The Science Behind Liposomal & Combination Approaches
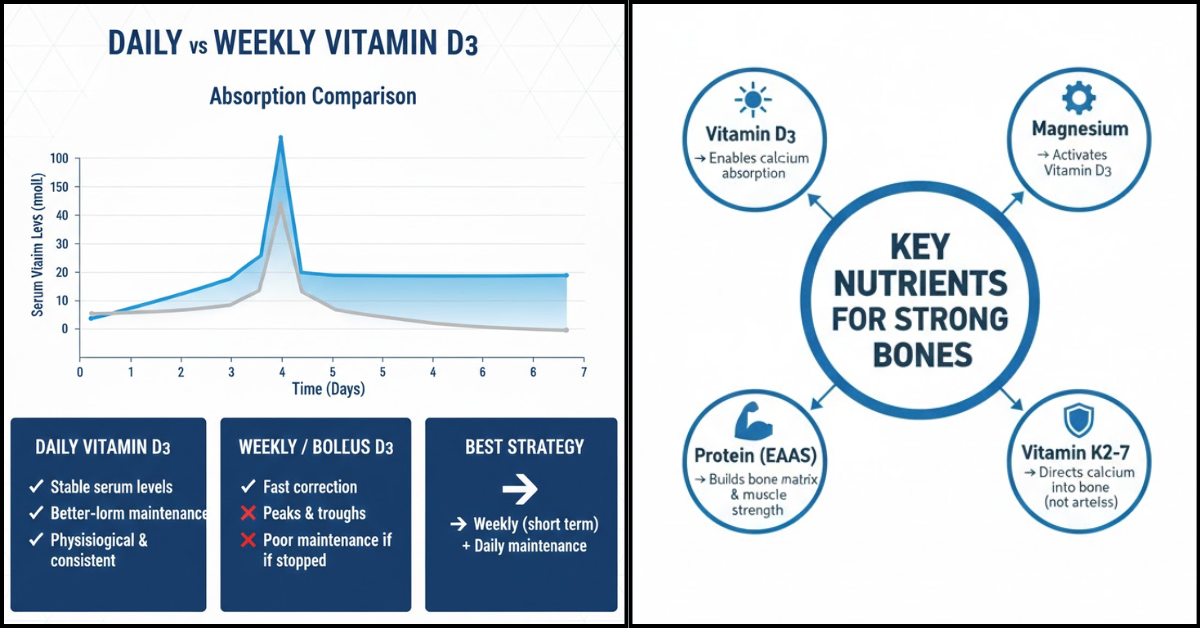
Liposomal Delivery: Why It Matters
Traditional oral supplements often face barriers such as:
- variable absorption due to fat-dependency
- gut health issues
- enzymatic degradation
Liposomal delivery encapsulates nutrients in phospholipids, facilitating direct cellular uptake and improved bioavailability.
For instance, liposomal vitamin D3 is better absorbed and more consistent in raising serum levels compared with conventional forms — a key advantage in populations with widespread absorption challenges due to lifestyle or comorbidities.
Cofactor Synergy: Magnesium & Vitamin D3
Magnesium is essential for the conversion of vitamin D into its active form and for bone matrix synthesis. Without adequate magnesium, vitamin D supplementation alone often yields suboptimal outcomes. Integrating liposomal magnesium with vitamin D3 ensures both improved activation and functional utilization.
Vitamin K2-7 Directional Calcium Usage
Vitamin K2-7 supports the activation of osteocalcin, a protein that helps bind calcium into bone rather than allowing it to deposit in arteries or soft tissue. This aspect is often overlooked but is critical as bone quality — not just quantity — determines fracture risk.
Precimax Formulations and the Vision for a Strong Nation
At a public health level, India needs a nutrition and bone health ecosystem that integrates evidence, technology, and preventive solutions. Here’s how Precimax’s advanced formulations align with this vision:
Formulation | Target Mechanism | Life-stage Impact |
Liposomal MGD3 | Magnesium repletion + co-factor support | Enhances vitamin D activation, muscular relaxation, neuromuscular function |
Liposomal Vitamin D3 | Improved absorption | Elevates serum 25(OH)D efficiently across ages |
Healobone | Micronized Cissus quadrangularis + D3 + K2-7 | Bone rejuvenation and mineralization support |
EAA MAX | High-strength whey protein | Supports muscle and bone matrix coupling |
MAXLITE | Metabolic support | Weight management improving mechanical loading on bone |
Why a Strong Bone Health Strategy Is Also a Strong Nation Strategy
Bone health is tightly linked to:
- mobility and independence in older adults
- reduced healthcare costs from fractures and falls
- quality of life and productivity
- reduced morbidity in chronic conditions
A society with robust bone health patterns is more productive and less burdened by years of disability.
Conclusion: A Call for Integrated Bone Health Action
The ETHealthworld NutriWell Conclave concluded with a unanimous message: Bone health must become a public health priority with interventions that span the lifecycle — from childhood to old age. Preventive care, evidence-based supplementation, lifestyle interventions, and nutraceutical support with scientifically advanced formulations can together build stronger bones and a stronger nation.
References & Citations
- ETHealthworld: “From Childhood to Old Age: Experts Call for a Lifelong Bone Health Strategy for India,” Economic Times HealthWorld (2026).
• Arch Osteoporosis 2025 study on lifestyle & bone health determinants India.
Sources:
https://health.economictimes.indiatimes.com/news/industry/from-childhood-to-old-age-experts-call-for-a-lifelong-bone-health-strategy-for-india/126433790
Experts Call for a Lifelong Bone Health Strategy for India
Experts Call for a Lifelong Bone Health Strategy for India
FAQ
Q: What’s the best way to dose vitamin D3 — daily or weekly?
A: Daily dosing offers more stable serum levels and better long-term maintenance.
Q: Why does vitamin D level drop after stopping weekly supplements?
A: Because weekly doses may not build sustained vitamin D reserves.
Q: Is liposomal vitamin D3 absorbed better?
A: Yes — liposomal D3 has enhanced cellular uptake independent of fat digestion.
Q: What serum level should we aim for?
A: 70–100 ng/mL for optimal bone health in chronic conditions.
Q: Why is magnesium important with vitamin D?
A: Magnesium is required for vitamin D activation and function.
Q: Can sunlight alone fix deficiency?
A: Usually not — lifestyle, diet, and supplementation are also needed.
Q: Do gummies correct deficiency?
A: Gummies may help fortify, but lack therapeutic absorption.
Q: Does obesity affect vitamin D response?
A: Yes — adipose tissue sequesters vitamin D and reduces availability.
Q: How often should vitamin D be tested?
A: Typically every 8–12 weeks after dose change, then annually.
Q: Can elderly take daily vitamin D safely?
A: Yes — especially with liposomal forms for better tolerance.
Q: Is calcium alone enough for bone health?
A: No — vitamin D, Mg, protein, K2 are also critical.
Q: Do bone fractures only affect elderly?
A: No — deficiency & poor bone density occur across ages.
Q: Why do some patients plateau despite supplementation?
A: Missing cofactors, poor adherence, or absorption issues.
Q: Does magnesium supplementation improve D3 response?
A: Yes — cofactor support enhances activation and effect.
Q: Can vitamin D help joint pain?
A: Yes — especially if deficiency is involved.
Q: Is weekly dosing still useful?
A: Yes — mainly for initial correction under guidance.
Q: What causes vitamin D toxicity?
A: Usually excessive unsupervised dosing, not typical supplementation.
Q: Should same lab be used for repeat tests?
A: Preferably yes — for trend accuracy.
Q: Can vitamin D3 support diabetes management?
A: Yes — it aids insulin sensitivity and metabolism.
Q: Why does vitamin D therapy fail?
A: Inefficient form, poor absorption, inadequate duration or dose.