Introduction: IBS is More Than “Acidity” — It’s a Gut–Brain–Microbiome Disorder
Irritable Bowel Syndrome (IBS) is one of the most common and frustrating digestive disorders affecting millions of Indians today.
It is characterized by:
- Bloating
- Abdominal discomfort
- Constipation or diarrhea
- Altering bowel patterns
- Gut sensitivity and stress linkage
IBS is not simply “gas” or “acidity.” Modern medicine recognizes IBS as a complex gut–brain–microbiome disorder, where gut bacterial imbalance plays a central role.
For many patients, lifestyle measures alone are not enough. Increasingly, clinical evidence supports that high‑strength probiotics and synbiotics can help restore gut balance and improve IBS outcomes.
So the key question becomes:
Which probiotic works clinically for IBS in India?
Let’s explore.
IBS in India: A Rapidly Rising Gut Health Challenge
IBS affects an estimated 10–15% of the global population, and India is seeing rising incidence due to:
- Urban diets high in processed foods
- Chronic stress and sleep disruption
- Frequent antibiotic exposure
- Low fiber intake
- Microbiome disturbances
IBS is now among the most common conditions seen in gastroenterology clinics, especially in adults aged 20–45.
Clinical Takeaway Box
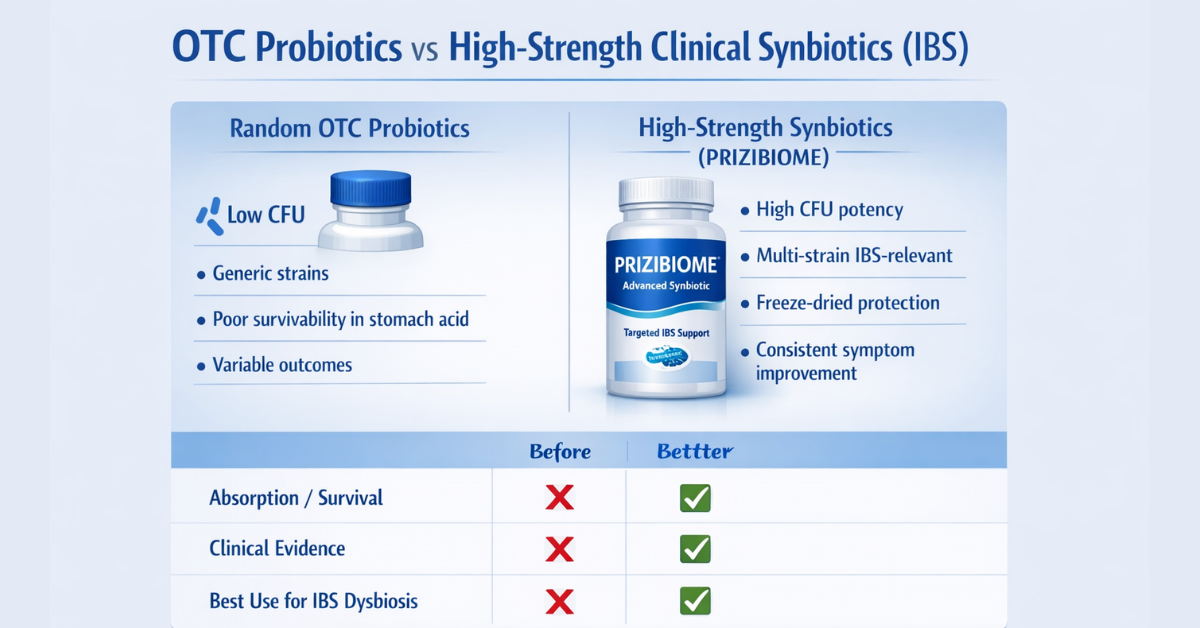
IBS improves with probiotics only when the strains are clinically relevant, CFU strength is high, and survivability through stomach acid is ensured.
Random low-dose OTC probiotics often fail.
Understanding IBS: Not One Condition, But Multiple Subtypes
IBS is not a single disease. It exists in subtypes:
1. IBS‑C (Constipation Predominant)
- Hard stools
- Infrequent bowel movements
- Straining and bloating
2. IBS‑D (Diarrhea Predominant)
- Loose stools
- Urgency
- Frequent episodes
3. IBS‑M (Mixed Type)
Alternating constipation + diarrhea
4. IBS‑U (Unclassified)
Each subtype has different microbiome patterns — which is why probiotic selection matters.
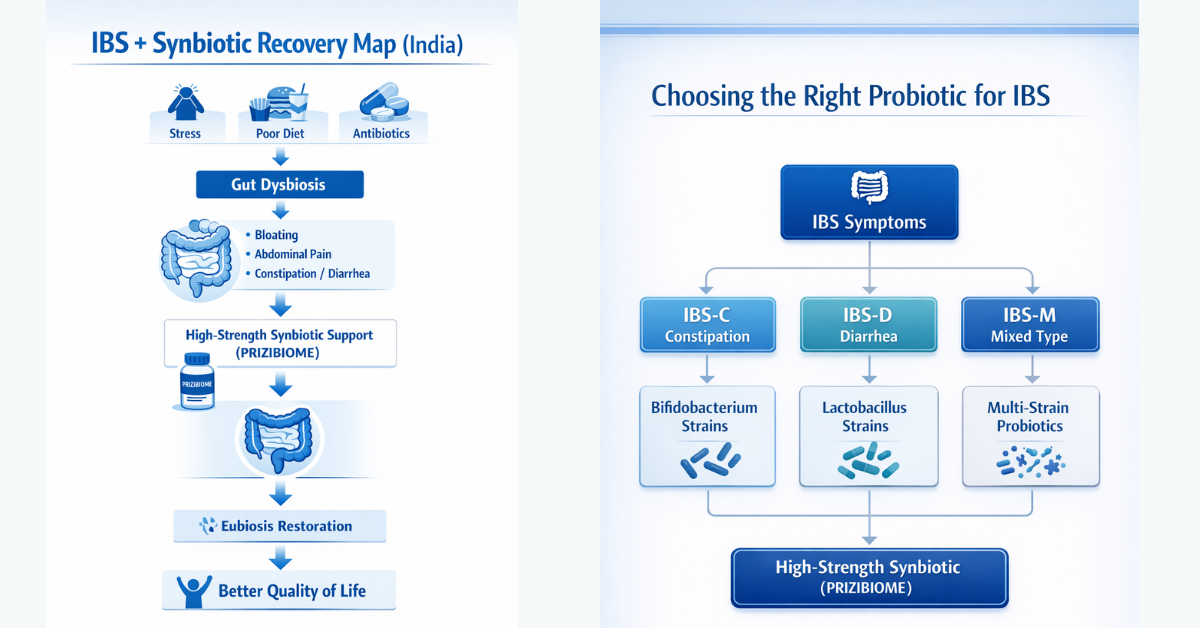
The Root Cause: Dysbiosis vs Eubiosis
Dysbiosis
An imbalance where harmful bacteria dominate beneficial microbes.
Dysbiosis leads to:
- Excess gas production
- Low-grade inflammation
- Altered gut motility
- Gut hypersensitivity
Eubiosis
A healthy microbiome state supporting:
- Proper digestion
- Immune regulation
- Barrier integrity
- Lower inflammation
The goal of probiotics is not just symptom relief — it is restoring eubiosis.
Probiotics vs Prebiotics vs Synbiotics
| Type | Meaning | Role in IBS |
|---|---|---|
| Probiotics | Live beneficial bacteria | Restore flora balance |
| Prebiotics | Fibers that feed probiotics | Support colonization |
| Synbiotics | Probiotic + prebiotic together | Stronger long-term IBS benefit |
Synbiotics often work best in IBS because they provide:
✅ immediate strain support + ✅ sustained microbial nourishment
Do Probiotics Really Help IBS? What Evidence Shows
Meta-analyses and post‑2020 reviews suggest probiotics help IBS by improving:
- Bloating
- Stool consistency
- Abdominal pain
- Quality of life
However, benefit depends on:
- Right strains
- High CFU potency
- Survivability through stomach acid
- Consistent daily intake for 4–8 weeks
Random OTC vs Clinically Designed Synbiotics
| Feature | OTC Probiotics | High‑Strength Synbiotics (PRIZIBIOME) |
|---|---|---|
| CFU strength | Low–moderate | High clinical potency |
| Strains | Generic single strains | Multi‑strain IBS relevant |
| Survivability | Poor in gastric acid | Freeze‑dried protection |
| Use case | General wellness | IBS dysbiosis correction |
| Predictability | Variable results | More consistent outcomes |
Which IBS Types Benefit Most?
IBS‑C
Probiotics may improve motility and reduce gas
Helpful strains: Bifidobacterium lactis
IBS‑D
Certain strains reduce diarrhea and inflammation
Helpful strains: Saccharomyces boulardii
IBS‑M
Multi‑strain synbiotic approaches perform best
Why CFU Strength Matters in IBS
IBS patients often need higher potency probiotics because:
- Dysbiosis severity is significant
- Antibiotic history is common
- IBS relapse is frequent
This is where advanced synbiotic formulations become clinically relevant.
Introducing PRIZIBIOME: High‑Strength Synbiotic Support
PRIZIBIOME (Precimax) is a next‑generation synbiotic designed for gut restoration.
Key advantages:
- High-strength probiotic + prebiotic combination
- Freeze‑dried survivability
- Multi‑strain clinically relevant spectrum
- Supports microbiome balance + IBS symptom relief
Especially relevant for:
- Chronic bloating
- Post‑antibiotic dysbiosis
- Constipation + incomplete evacuation
- Mixed IBS patterns
Expert Comments from Clinical Practice
Dr. Ramesh, Vijayawada
“In IBS patients with chronic bloating and post-antibiotic imbalance, high‑strength synbiotics have shown meaningful improvement.”
Dr. Vimala Rani, Mysore
“We increasingly recommend synbiotic probiotics alongside diet modification for better stool regulation and reduced discomfort.”
Diet Strategies That Enhance Probiotic Outcomes
Low‑FODMAP Diet
Reduces fermentable carbs that worsen bloating.
Gradual Fiber Introduction
Helpful in IBS‑C (psyllium, oats).
Avoid Unnecessary Antibiotics
Antibiotics worsen dysbiosis.
When to Consult a Gastroenterologist (Important)
Seek medical attention if IBS is accompanied by:
- Weight loss
- Blood in stools
- Persistent fever
- Severe diarrhea
- Symptoms >3 months unresponsive
- Family history of IBD/cancer
Conclusion: IBS Management Requires Microbiome Restoration
IBS is not just acidity — it is a gut–brain–microbiome disorder.
The future lies in restoring eubiosis through:
- Clinically validated strains
- High CFU potency
- Synbiotic formulations
- Diet + lifestyle integration
PRIZIBIOME represents an evidence‑aligned synbiotic option for IBS symptom support in India.
Frequently Asked Questions (FAQs)
A high-strength multi‑strain synbiotic with clinical CFU, such as PRIZIBIOME.
IBS is chronic, but probiotics can significantly reduce symptoms and relapse frequency.
Most patients need 4–8 weeks of daily use.
Yes, synbiotics combine strains + prebiotic support for longer benefit.
Bifidobacterium-based strains improve motility and stool softness.
Saccharomyces boulardii is often useful for diarrhea-predominant IBS.
Yes, mild gas may occur in week 1 as the microbiome adapts.
An imbalance where harmful bacteria dominate beneficial microbes.
A healthy, balanced microbiome state.
Yes, consistency is key for symptom improvement.
Yes, synbiotics are safe when quality-controlled.
Yes, but should be introduced gradually as excess may increase gas.
Yes, IBS is a gut–brain axis disorder.
IBS is functional, but low-grade microbiome inflammation is common.
No, they complement standard care.
Yes, they are especially important post-antibiotic dysbiosis.
Low‑FODMAP and fiber-balanced diets improve outcomes.
IBS typically needs higher CFU multi‑strain products.
No, strains and survivability determine clinical success.
Evidence and clinical adoption suggest yes.